iMEDS: Automated Sedation Assessment in the PICU
- Feiyang Huang
- Barbara Pejic
- Sayantika Roy
- Audrey Lacy
- Junseong Park
- Sidharth Raghavan
- Jake Hoffman
- Tanvi Ranade
- Dr. Nicholas Durr (Faculty mentor)
- Dr. Sapna R. Kudchadkar (Clinical mentor)
- Dr. James C. Fackle (Clinical mentor)
- Dr. Sandya Subramanian (Committee member)
- Dr. Chinyere Egbuta (Committee member)
- Kim Hwang Yeo (Teaching assistant)
Abstract:
Among 250,000 children receiving pediatric critical care in the United States annually, more than 90% receive sedatives. Of these, 42% receive improper sedative doses, which lead to adverse outcomes and prolongs PICU stay. This creates an enormous burden for healthcare systems as sedation accounts for 40% of the variability in cost of care in the ICU. Sedation assessments by nurses are typically used to inform sedation decisions, but they increase the nursing burden and result in highly variable outcomes. Against this backdrop of high adverse event rates and the healthcare labor shortage, there is a need to automatically and accurately evaluate patient sedation-agitation state in order to inform dosage decisions.
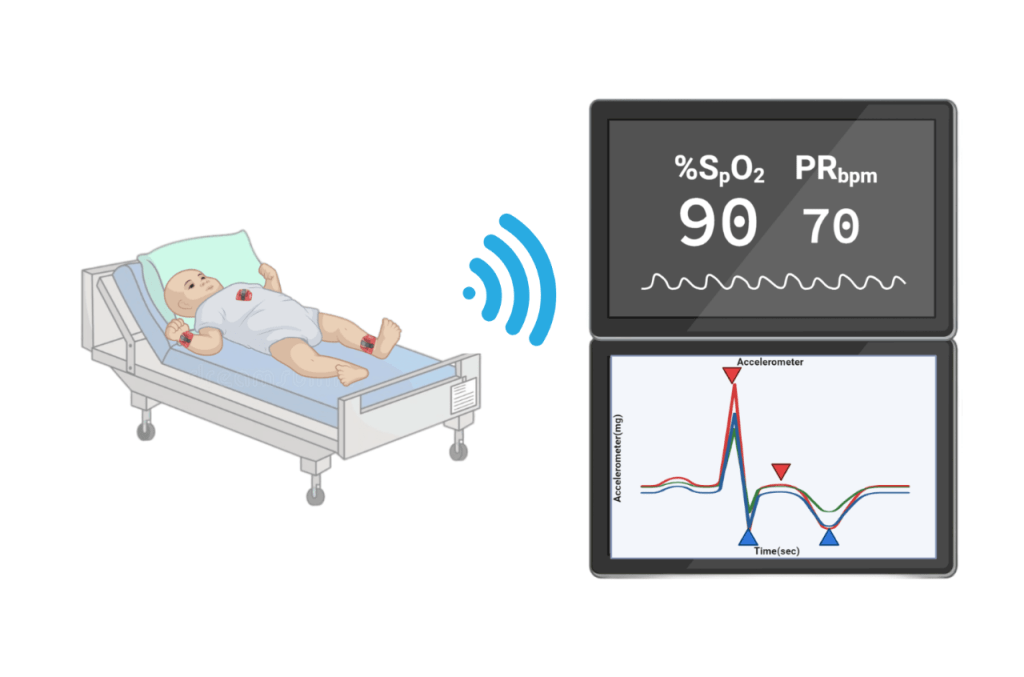
Multiple input factors are used in sedation assessment including chest heaving, twitching, extubation and response to noxious stimuli. Multimodal vital time-series data from existing ICU monitors can potentially capture signals that correlate to these events. Accelerometry has also been shown to detect postoperative anesthetic events earlier than other physiological markers. While these data are difficult to interpret in clinical practice, recent advancements in machine learning have demonstrated better performance at managing sedation in adult ICU than critical care clinicians. Therefore, machine learning and sensor technology have the potential to enable precision medicine in pediatric ICU sedation.
We propose a medical device that measures a patient’s accelerometry and combines it with other vital signs measured in the ICU. A machine learning algorithm will be trained to infer patient sedation state using these multimodal signals. This can potentially create a new paradigm of continuous monitoring, consistent assessment and predictive care planning in pediatric sedation management.