Designing a Novel Port System to Reduce Membrane Rupture in Fetal Therapy Procedures
- Selena Shirkin
- Mariah Snelson
- Eric McAlexander
- Daniel Lewis
- Jonathan Wu
- Ayeeshi Poosarla
- Gloria Kalnitskaya
- Alice Yu
- Elizabeth Logsdon (Faculty mentor)
- Dr. Ahmet Baschat (Clinical mentor)
- Dr. Jena Miller (Committee member)
- Dr. Mara Rosner (Committee member)
- Dr. Michelle Kush (Committee member)
- Dr. Geoffrey Miller (Committee member)
- Bhavya Gopinath (Teaching Assistant)
Abstract:
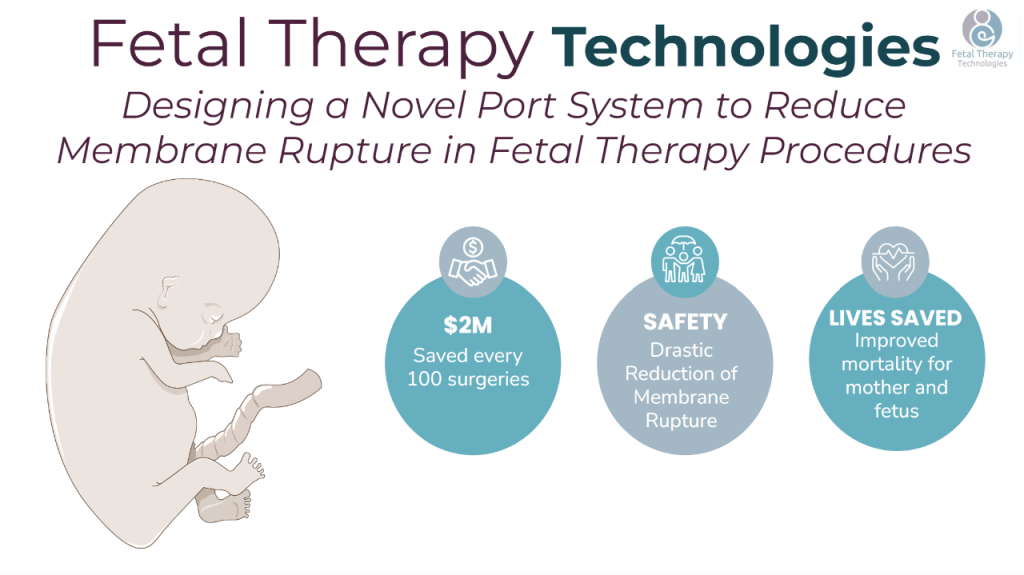
Fetal therapy is a minimally invasive endoscopic procedure performed on a pregnant person to surgically correct prenatal birth defects with a single port inserted through the abdomen and into the uterus. The highest risk associated with fetal therapy is amniotic membrane rupture, which leads to premature delivery and occurs in about 30-40% of fetal interventions. When an entry port is inserted into the uterus, it pierces through the uterine wall and the amniotic membrane. After surgery, a permanent hole is left in the amniotic membrane as this tissue lacks self-healing abilities. Previous research suggests that amniotic fluid can leak out of this hole and cause the amniotic membrane to separate from the uterine wall, inducing membrane rupture and preterm labor. This port-site failure occurs because Maternal-Fetal Medicine specialists lack port system instrumentation designed for the uterine environment. High rates of membrane rupture may be reduced using tools optimally designed for fetal therapy (Baschat 2022). Thus, we have designed a novel port system that is optimized for the uterine environment. Our technology easily incorporates into the current clinical workflow, prevents amniotic fluid leakage between the amniotic membrane and uterine wall, and mitigates amniotic membrane damage or tearing during surgery. With improvements to the method of accessing the uterus, rates of amniotic membrane rupture and preterm delivery can be significantly reduced across a variety of conditions. This innovation has the potential to impact all fetal interventions by drastically reducing complication rates, saving countless lives, and minimizing hospital expenditures.