So Long, Trial and Error
If you have ever traveled in a modern jetliner, crossed a bridge, or ridden in a car, you’ve entrusted your life to computer simulations. Such models are used to design everything from aircraft and bridges to automobiles and buildings, making sure they are as safe as possible. But when it comes to designing treatments for patients with serious and even life-threatening conditions, physicians often rely on an approach best described as “trial and error.”
My research is dedicated to changing that. With my team, I am working to bring the precision of computer simulations to clinical practice so we might help physicians make the best possible treatment decisions for every patient. I believe that such models are poised to transform medicine, heralding the arrival of a new brand of personalized health care and dramatically improving patient outcomes.
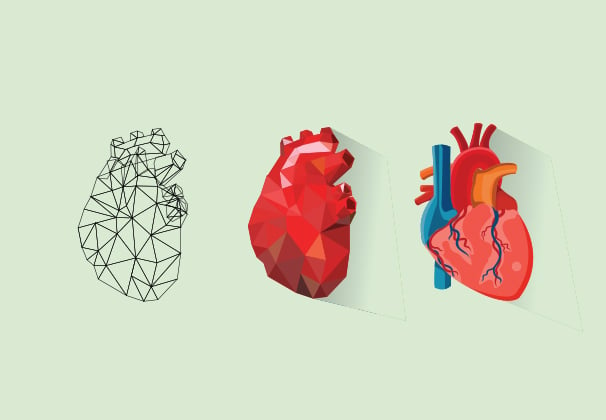
In my lab, we are doing this through the creation of sophisticated 3-D “virtual hearts”—models that enable cardiologists to test lifesaving interventions. Doctors can poke and prod these virtual organs in ways that are simply not possible with flesh-and-blood hearts. Clinicians not only minimize the invasiveness of diagnostic procedures but also—and most importantly—improve therapies.
One of our projects provides an example. Using MRI images, we have created detailed models of the hearts of patients who had survived heart attacks but were left with damaged tissue that predisposes their hearts to deadly arrhythmia. This is a condition in which the heart’s electrical signals run amok, causing irregular and abnormal rhythms that can result in sudden death.
Current treatment involves implanting a small device called a defibrillator that can sense the onset of an abnormal rhythm event and shock the heart back to its normal pace. This invasive procedure carries numerous risks, including infections and heart tissue damage, so it is important that only patients who need the device get it.
So how do doctors determine which patients actually need defibrillators? They use something called the “ejection fraction,” a measure of the amount of blood pumped out of the heart with each beat. If that number is less than 35 percent, then the patient is considered at high risk of sudden cardiac death by arrhythmia and warrants an implant.
The trouble is that ejection fraction is not a good predictor of the patient’s risk of dying suddenly, because it takes into account only blood flow and doesn’t consider the heart’s electrical activity. Using only blood flow to predict who will experience a life-ending arrhythmia episode is like having an electrical problem in your house and calling a plumber to fix it. As a result, many patients get defibrillators that they don’t really need. Worse yet, this inaccurate criterion means that many patients who are at risk of suffering arrhythmias don’t get the devices they need.
Our personalized virtual hearts could help doctors make better decisions in these cases. These digital replicas allow us to factor in not only the unique geometry of each patient’s individual heart, but also the impact of the heart-attack-related scar tissue and the pattern of electrical waves as they move throughout the organ.
We have demonstrated that this method, called VARP (virtual-heart arrhythmia predictor), significantly outperforms any other current approaches for predicting which patients are at risk of arrhythmias. It has the potential to save lives, and also to save patients from getting defibrillators they don’t need.
We look forward to a time when all heart patients, from babies to senior citizens, have virtual hearts, which doctors can then use to plan their personalized treatment. The pursuit of this merger of computational simulation and clinical medicine is the future of medicine.
– Natalia Trayanova
