A new AI model is much better than doctors at identifying patients likely to experience cardiac arrest.
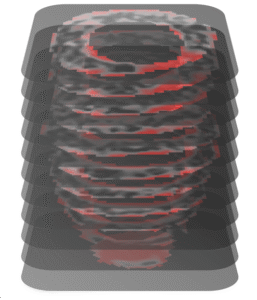
The linchpin is the system’s ability to analyze long-underused heart imaging, alongside a full spectrum of medical records, to reveal previously hidden information about a patient’s heart health.
The federally funded work, led by Johns Hopkins University researchers, could save many lives and also spare many people unnecessary medical interventions, including the implantation of unneeded defibrillators.
“Currently we have patients dying in the prime of their life because they aren’t protected and others who are putting up with defibrillators for the rest of their lives with no benefit,” said senior author Natalia Trayanova, a researcher focused on using artificial intelligence in cardiology. “We have the ability to predict with very high accuracy whether a patient is at very high risk for sudden cardiac death or not.”
The findings are published today in Nature Cardiovascular Research.
Hypertrophic cardiomyopathy is one of the most common inherited heart diseases, affecting one in every 200 to 500 individuals worldwide, and is a leading cause of sudden cardiac death in young people and athletes.
Many patients with hypertrophic cardiomyopathy will live normal lives, but a percentage are at significant increased risk for sudden cardiac death. It’s been nearly impossible for doctors to determine who those patients are.
Current clinical guidelines used by doctors across the United States and Europe to identify the patients most at risk for fatal heart attacks have about a 50% chance of identifying the right patients, “not much better than throwing dice,” Trayanova says.
The team’s model significantly outperformed clinical guidelines across all demographics.