Solving the paradox: How one bad apple spoils the pie of cardiac rhythms
The redundancy of genes encoding for critical proteins guarantees survival. For example, a ubiquitously expressed calcium sensor molecule, calmodulin — vital to heart and muscle contraction, memory, and immunological responses — is encoded by three different genes. However, this biological safeguard fails in a growing number of patients discovered over the past two years to be afflicted with so-called ‘calmodulinopathies.’ Here, de novo mutations in only one of six alleles of calmodulin genes render life-threatening cardiac arrhythmogenic events. But, how does an abundance of wild-type calmodulin get overpowered by something as rare as one-in-six sighting of mutant calmodulin?
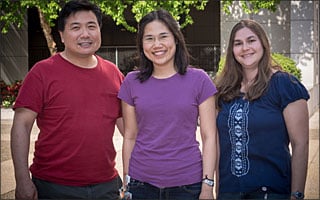
Worawan (Boombim) Limpitikul (MD-PhD candidate), Ivy E. Dick (Postdoctoral Fellow), and Professor David T. Yue from Calcium Signals Laboratory in the Biomedical Engineering and Neuroscience Departments, exploit live-cell biochemistry, electrophysiology, and mathematical simulations to solve this paradox of how one bad apple can spoil the pie of normal cardiac rhythms. This work, Calmodulin Mutations Associated with Long QT Syndrome Prevent Inactivation of Cardiac L-type Ca2+ Currents and Promote Proarrhythmic Behavior in Ventricular Myocytes, was just published online in the Journal of Molecular and Cellular Cardiology.
By introducing the corresponding mutant calmodulins into adult cardiac ventricular myocytes, the Hopkins team not only produced a cellular version of the disease phenotypes found in patients, but also identified a major molecular target of these mutant calmodulins, namely the L-type calcium channels in the surface membrane of heart cells.
These channels not only furnish the calcium ion influx that initiates the heartbeat, they also dictate the duration of the electrical event accompanying this contractile event. Because of these critical functions, the opening of these channels is feedback controlled by calmodulin, a calcium sensor that throttles down channel opening upon calcium elevation. The Hopkins investigators found that the mutant calmodulins substantially reduced this feedback control, thereby creating abnormally long heart beats.
By exploiting deep basic knowledge of how calmodulin interacts with L-type channels, together with innovating live-cell biochemical techniques and mathematical simulations, the team was able to explain how a limited amount of mutant calmodulin could have significant effects on feedback control. Because even the calcium-free form of calmodulin is pre-bound to L-type calcium channels, and mutant calmodulins are only defective in their ability to bind calcium, channels will affiliate with mutant calmodulins in proportion to their approximately one-in-six prevalence. However, once calcium rises near channels paired with a defective calmodulin, no down throttling of opening occurs in these channels, and this effect suffices to induce abnormally long heart beats.
Using newly devised biochemical and electrophysiological tools, the team quantitatively confirmed this mechanism, furnishing means to predict the severity heartbeat disruption based on the prevalence of mutant calmodulin. In this era of personalized medicine, basic mechanisms such as this are required to gauge the level of genetic amelioration of mutated genes needed to restore patients to normal cardiac rhythms.
